
Liver transplantation is a critical surgical procedure that replaces a diseased or failing liver with a healthy liver or a portion of one from a donor. It is often a life-saving solution for individuals suffering from severe liver diseases such as cirrhosis, acute liver failure, and certain types of liver cancer. There are two main types of liver transplants: deceased donor liver transplantation (DDLT), where the liver is sourced from a deceased individual, and living donor liver transplantation (LDLT), where a healthy portion of a liver is donated by a living person. In both scenarios, the liver regenerates to near-normal size in both the donor and the recipient. When considering a liver transplant, one important factor to take into account is the Liver Transplant Cost In India, which is more affordable compared to many other countries, making it a popular destination for medical tourism. The cost varies based on factors like hospital, type of transplant, and the patient’s individual case, but it offers a valuable option for those in need of this life-saving treatment.
The liver is a large, reddish-brown organ located in the upper right abdomen beneath the diaphragm. It is the largest internal organ in the human body, weighing approximately 1.4–1.6 kilograms in adults. The liver is divided into two main lobes, the right and left lobes, which are further subdivided into smaller lobes.
Composed primarily of specialized cells called hepatocytes, the liver plays a central role in metabolism, detoxification, and digestion. Hepatocytes process nutrients absorbed from the digestive tract, store energy in the form of glycogen, and produce bile, a fluid essential for fat digestion. The liver also detoxifies harmful substances, metabolizes drugs, and synthesizes important proteins, including blood-clotting factors and albumin.
The liver receives blood from two sources: oxygenated blood from the hepatic artery and nutrient-rich blood from the portal vein. Its regenerative capacity is remarkable, enabling it to recover from damage or partial removal.


The liver excretes bile serum and regulates the bulk of blood chemical levels. This facilitates the liver’s ability to eliminate waste. All of the blood that exits the stomach and intestines is filtered by the liver. The liver processes blood, converting drugs into forms that are safer for the body or simpler to utilize, as well as breaking down, balancing, and producing nutrients. The liver is in charge of more than 500 crucial processes. Some of the most well-known functions include the following:
A viral infection that can lead to chronic liver inflammation, scarring (cirrhosis), and liver cancer. Prolonged damage from untreated hepatitis B often results in liver failure, necessitating transplantation.
Another viral infection causing chronic inflammation and significant liver damage. It is a leading cause of cirrhosis and hepatocellular carcinoma, which may require liver transplantation as a final treatment.

Chronic and excessive alcohol consumption can lead to conditions like alcoholic hepatitis or cirrhosis. Once the liver is severely scarred and non-functional, a transplant may be the only life-saving option, provided the patient abstains from alcohol for a specified period.
NASH is an advanced form of non-alcoholic fatty liver disease (NAFLD) where inflammation and liver cell damage occur due to fat accumulation. These conditions can progress to cirrhosis or liver failure, making transplantation necessary.
A condition where the immune system mistakenly attacks the liver, leading to inflammation and damage. If untreated or unresponsive to medication, it can cause cirrhosis and liver failure, making transplantation necessary.

A rare genetic disorder where copper accumulates in the liver and other organs, causing toxicity. Advanced cases may lead to liver failure, which requires a transplant to remove the damaged organ.

In cases where a previous transplant fails due to organ rejection, infection, or other complications, a second transplant (re-transplantation) may be required.

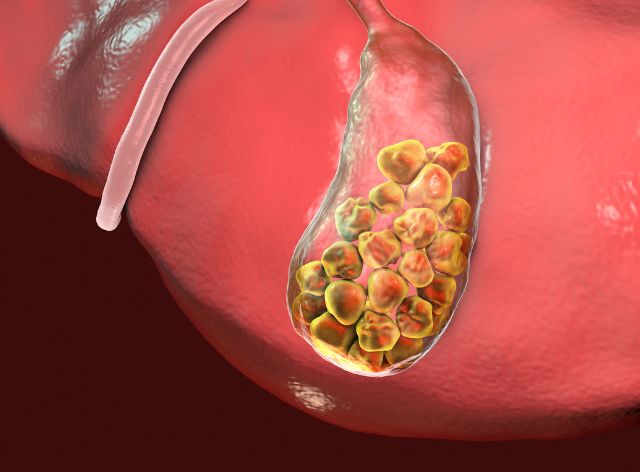
A rare inherited disorder where multiple cysts form in the liver, causing enlargement and impaired function. In severe cases, where symptoms and complications are debilitating, a liver transplant is the only effective treatment.
A genetic disorder causing excessive iron buildup in the liver, leading to tissue damage and cirrhosis. When liver function is significantly impaired, a transplant becomes necessary.

Hepatocellular carcinoma (HCC) is the most common liver cancer and can sometimes be treated with a transplant. Other tumors, if localized and within specific criteria, may also qualify for transplantation.
An autoimmune condition that damages the bile ducts in the liver, leading to inflammation and scarring. Transplantation is considered when it progresses to liver failure.

Sudden and severe liver dysfunction, often caused by drug toxicity (e.g., acetaminophen overdose), infections, or autoimmune conditions. In critical cases, a liver transplant is the only life-saving option.
The cost of liver transplantation in India is influenced by several factors, including hospital infrastructure, surgeon expertise, and the type of transplant (deceased or living donor). On average, the procedure costs between ₹20-30 lakhs ($25,000-$40,000), significantly lower than in Western countries. Expenses include pre-transplant evaluations, surgery, post-operative care, and lifelong immunosuppressive medications. Costs may rise with complications or prolonged hospital stays. Government schemes and charitable organizations help reduce financial burdens for eligible patients. Despite its affordability compared to global standards, the procedure remains inaccessible for many due to India's socioeconomic disparities and limited public healthcare funding.
Liver transplantation in India is influenced by organ availability, financial constraints, and healthcare accessibility. The low deceased organ donation rate, due to cultural beliefs and lack of awareness, creates a reliance on living donors. The high cost, averaging ₹20-30 lakhs, limits access for many, despite government and NGO support. Geographic disparities in healthcare infrastructure mean advanced facilities and skilled surgeons are concentrated in urban centers, leaving rural populations underserved. Additionally, regulatory frameworks and ethical concerns surrounding organ allocation can impact fairness. Public awareness campaigns, improved donation systems, and expanded healthcare access are vital to addressing these challenges effectively.
Liver Transplantation have emerged as one of the most effective medical advancements during the preceding 50 years. This medical therapy is currently in its golden age in India as a result of the rise in surgical operations and technological breakthroughs over the past few decades. Contact our expert to learn more about inexpensive liver transplant price in india.
India has grown to be one of the most sought-after locations for medical tourism worldwide because of these figures and the fact that Indian team physicians are knowledgeable about the most recent advancements in the healthcare sector. Contact us now for how much liver transplant cost in India ? The price of liver transplant in India varies widely, depending on factors like the hospital, location, and medical team. On average, it can range from $35,000 or about INR 24,50,000., making India an affordable destination for high-quality liver transplants, attracting patients from around the world seeking cost-effective healthcare solutions.

Many factors persuade people to pick liver transplant cost India for their medical care. The quality of healthcare services is another factor, in addition to the price disparity.
Innovations in liver transplantation have significantly improved outcomes and expanded accessibility. Advanced surgical techniques, such as living donor and split liver transplantation, maximize organ availability. Enhanced immunosuppressive therapies reduce rejection rates while minimizing side effects. Organ preservation technologies, like normothermic machine perfusion, maintain donor liver viability during transport. Minimally invasive approaches and robotic-assisted surgeries are refining recovery and reducing complications. Research in regenerative medicine, including stem cell therapy and bioengineered livers, offers future alternatives to transplantation. Additionally, xenotransplantation (using animal organs) and gene editing are being explored to address organ shortages, paving the way for breakthroughs in liver failure treatment.
In liver transplant hospital in India, more than 80% of liver transplants from living donors take place, as opposed to western regions where around 90% of transplants come from dead donors.
If the person is brain dead, he is considered to be dead and is going to have his liver transplanted. The liver has been donated to the necessary patient on the waiting list after fitting the deceased person’s blood type and measurements. Since the liver has the ability to regenerate, it is periodically split into two halves and transplanted simultaneously into two patients—a child and an adult.
It is a living donor transplantation if a liver lobe has been removed from a healthy donor and implanted into the recipient to replace the sick liver. The donor must be a close relative, such as a parent, grandparent, kid, spouse, or grandchild. When the liver is split or transplanted, the liver begins to regenerate and expand to its normal size. Their entire liver must regenerate to its original size over the course of two to three weeks.
Given that the liver donation is an organ donation, both the donor and the recipient must abide by all laws and regulations set out by the Indian government. You can contact us for liver donation price in india & procedure.

Being treated requires taking a big step, and having a positive outlook is important. The exam is a sequential process that begins with the receiver’s assessment. Based on their own blood supply, the household begins its hunt for donors once the person is eligible for transplantation.
If the donor is found, the transplant procedure typically takes around two to three weeks after the consent committee has given its approval.
Post-surgery management is crucial for the success of liver transplantation, focusing on preventing organ rejection, infections, and complications. Patients require lifelong immunosuppressive medications to suppress the immune response and protect the new liver. Regular follow-ups monitor liver function, detect early signs of rejection, and manage side effects of medication. A balanced diet, hydration, and gradual physical activity support recovery. Psychological support is essential to address emotional and lifestyle adjustments. Common complications like infections, bile duct issues, or recurrence of liver disease are managed promptly. Adherence to medical advice and close monitoring ensure long-term graft function and improved quality of life.

Out of concerns and problems, there are two major issues that require attention:
Being the best advisors, we host reputable resources for patients looking for doctors, hospitals, and specialty therapies in India. For you, we’ll identify the best medical options. Our team will provide you with a list of licensed, recognized, and trusted physicians and medical facilities in relation to your medical needs. Additionally, we provide a cost-effective treatment plan. Aside from being the Best Advisers in India, we also help patients with a wide range of other services, like getting travel permissions and medical visas. Just visit our website to know more about how much cost for liver transplant in india? Do To know more you can follow us on Facebook.
The most common and clinically important side effects are biliary issues, fluid collections, neoplasms, and graft rejection. Arterial and venous thrombosis and stenosis are also common.
65-year-old or older people having severe disease. Significant organ damage has been caused by diabetes, excessive obesity, serious and aggressive liver illness, and hepatitis B.
If you are rejected, you could go through some mild symptoms, however other people might feel OK at first. The most typical early symptoms are fatigue, a temperature exceeding 100° F or 38° C, increased liver function examinations, yellowing of the eyes or skin, as well as a fever.
Common adverse effects of post-transplant drugs include increased blood pressure, altered mood, hair loss or growth, high blood sugar, bone and muscular weakness, renal malfunction, dizziness, puking, diarrhea, and migraine.
Normal liver transplant recovery times range from six to twelve hours. The liver will be excised during the treatment and transplanted with a donor’s liver. Due to the complexity of a transplant, many tubes will need to be inserted into your body.
On average, liver transplant recipients experience a five-year survival rate of approximately 75%. This means that out of every 100 individuals who undergo a liver transplant, approximately 75 can expect to live beyond five years, while around 25 may face mortality within this timeframe.
Indian Health Adviser (IHA) is a healthcare facilitator seeking to make health and wellness easier for people of international residents, their families, and their friends.
Designed by Acmeinfolabs